How to calm down hot flushes if you are going through the menopause
Hot flushes are thought to be caused by hormonal fluctuations—these are the best ways to ease them...


Hot flushes—also known as hot flashes—are one of the main symptoms of the menopause, alongside night sweats, mood changes, and reduced sex drive. In fact, eight in 10 women experience them for an average of seven years. While they are completely normal, and down to natural hormonal fluctuations at this time of life, they can be both uncomfortable and debilitating.
A lot has changed when it comes to how women manage symptoms caused by the menopause—and there are now even dedicated support groups for the sharing of useful advice. What's more, along with night sweats, hot flushes are one side-effect of this stage of life that is now being approached in a different way. Indeed, you no longer have to suffer in silence, and can make use of a number of solutions—from HRT to diet and alternative therapies. We've called on the experts to explain which lifestyle changes are best to make, as well as the common triggers to watch out for...
What are hot flushes and when do they begin?

If you're of menopausal age—usually between 45 and 55 years old—and are finding that you need to suddenly fling open the window or wake up drenched in sweat, then you could be experiencing hot flushes. They vary from woman to woman, but are usually recognizable as a sudden, creeping feeling of intense warmth or heat. They can often come from nowhere and quickly spread through the face, neck, chest and body. Sweating, palpitations and dizziness may accompany them too.
Hot flushes tend to start with the onset of the menopause. "The average age of this is 51," says Dr Louise Newson, a GP and author of Menopause (£9.74, Haynes). Genetics, underlying medical conditions and treatment for cancer could cause the menopause to begin early, which is defined as being before the age of 45. The menopause is preceded by the perimenopause, and it is also possible to experience hot flushes during this stage too.
"Hot flushes can last anything from a matter of seconds or up to an hour," notes Dr Newson. For some women they’re mild, but others report that their flushes make them feel like they’re trapped in a furnace. They can disrupt routines and knock confidence levels. However, it's worth noting that while they are a common menopausal symptom, they can also occur for other reasons.
How often is normal? Every woman will experience menopausal symptoms differently. This means there’s no ‘normal’ when it comes to the frequency of hot flushes. Having between five and ten flushes a day is considered to be average. However, some women may suffer from more than this, while others will report having none at all.
What causes hot flushes? The 3 main culprits

1. Alcohol
Drinking causes the blood vessels to expand in the body and the increased blood flow in through the vessels can make you feel hot and cause the skin to flush. All types of alcohol can bring on one—but red wine, in particular, is a known trigger. Sweating is also common with a hangover, so drinking may also worsen night sweats too.
Sign up to our free daily email for the latest royal and entertainment news, interesting opinion, expert advice on styling and beauty trends, and no-nonsense guides to the health and wellness questions you want answered.
To minimize the effect of alcohol on menopausal symptoms, it could be advisable to switch to drinks with a low-alcohol content or drink spritzers to reduce your intake. Mindful drinking is another way to cut back on your units.
2. Spicy food
Some food ingredients and spices can bring on a hot flush. This is due to a ‘fiery’ food compound called capsaicin that is found in peppers and chili powder.
3. Caffeine
A cup of coffee may leave you feeling alert and raring to go, but it could also cause a hot flush. That's because caffeine speeds up the heart rate, so blood is pumping through the body faster, leading you to feel hotter. Rely on your daily cuppa as an energy boost? There could be something else going on if you frequently feel tired in winter.
Other common triggers include:
- Hot food and drinks
- Smoking
- Stress
- Tight clothing
- Hot baths
- Using a hairdryer
Identifying and steering clear of your own ‘triggers’ can help to reduce the frequency and severity of your flushes.
How can you treat hot flushes?

Hormone replacement therapy
Often the first line of treatment for women suffering from menopausal symptoms, hormone replacement therapy—often known as HRT—could be an option. One US study found that low-dose estradiol, which is a form of estrogen, helped to reduce hot flushes by 50%.
Other types of HRT include combined HRT patches, which contain an effective duo of estrogen and progestogen. Speak to your doctor to find out if it’s the right option for you.
Other medications
If you don’t want to take HRT, other prescription medicines—including certain antidepressants and clonidine (usually prescribed to help with blood pressure)—might help.
Stay cool
Heat triggers flushes for some women. Using a fan and taking cooler baths and showers may help. You could also try cooling gels or placing a cold compress on the back of your neck when you feel one coming on.
Cultivating a good bedtime routine is important too. Wear layered clothing and switch your duvet for layers of sheets. And, strange as it sounds, some women wear socks to bed because it helps to lower their core body temperature.
Reduce stress
Keeping your stress levels down is often easier said than done, but it can really help. Try relaxing with one of the best meditation apps. Some women also do slow, deep abdominal breathing to ease symptoms—and it can be worth doing 15 minutes in the morning and evening, as well as when a hot flush starts, to help control the severity. Yoga for beginners and tai chi may also help.
Eat well
Phytoestrogens are found in plant foods like soy beans, chickpeas, lentils, ground flaxseed and red clover. These natural compounds have a similar chemical makeup to estrogen, and as a result, there's some evidence that eating foods rich in phytoestrogens can help to reduce the frequency and severity of hot flushes.
Women’s health specialist Dr Sally Moorcroft suggests eating green vegetables daily, since they’re packed with magnesium. She also advises drinking kefir for gut health, explaining: "A happy gut leads to less inflammation in the body, which can reduce your symptoms." The adaptogenic herbs ashwagandha and tulsi may help to reduce the effects of stress on the body and ease flushing.
Supplements for hot flushes
You could also try taking non-prescription medication and supplements for the menopause to help ease symptoms...
Folic acid: Taking 1mg of folic acid a day has been found to reduce the severity, duration and frequency of hot flushes
Vitamin E: Taking 400IU of vitamin E a day has likewise been found to help ease hot flushes
Ibuprofen: Some women find that taking an anti-inflammatory, non-steroidal painkiller relieves their hot flush symptoms
Complementary therapies for hot flushes
Hypnosis
It may seem like an unusual solution, but hypnosis can help hot flushes and night sweats. “It may also be beneficial for anxiety or low mood that accompanies them,” says Dr Caroline Houlihan-Burne, clinical hypnotherapist at The Princess Grace Hospital.
Want to try it at home? “Close your eyes, breathe deeply and count down from 10 to one on each 'out breath'," explains Dr Houlihan-Burne. "Repeat a positive suggestion in your mind, such as ‘I’ll remain cool and calm all day’. When you’re ready to come out of self-hypnosis, count from one to 10. On the count of 10, your eyes will open and you’ll come out of the trance."
Cognitive behavioral therapy
Cognitive behavioral therapy—or CBT—is a form of talking therapy. It identifies negative thought patterns to create positive changes in feelings and behavior. It’s particularly effective during the menopause, explains clinical psychologist Professor Myra S Hunter.
“CBT has been found to help women handle hot flushes and night sweats, as well as improve mood, sleep and quality of life,” explains Professor Hunter. Talk to your doctor about whether it may be suitable for you.
Acupuncture
A study found that women given 15-minute sessions of acupuncture weekly, for five weeks, were significantly less troubled by hot flushes.
So, how does it work? Mark Bovey, head of research at the British Acupuncture Council, explains: “Acupuncture’s effect on neurotransmitters linked to pain relief and mood regulation may influence the thermoregulatory center in the hypothalamus region of the brain.”
What else?
- Black cohosh—this herbal medicine is in the same plant family as the buttercup and is used by some women to help hot flushes and night sweats.
- Isoflavones—these are a type of phytoestrogens similar to natural estrogen and are found in red clover. Some women take them to reduce hot flushes, but they are not recommended if you have a history of breast cancer.
- Don quai, evening primrose oil or kava—they have also been used by women to treat hot flush symptoms, but there’s currently little evidence to support their effectiveness. Always talk to your doctor before trying a complementary medicine. Some may interfere with other medications or cause side effects.

TheraPearl cooling neck wrap
Cold therapy packs can reduce the severity of a hot flush—keep this gel-bead cold compress in the fridge for instant relief when one strikes.

Anti-Flush short sleeve night dress
This super-soft night dress boasts anti-flush technology to cool the skin and wick away moisture while you sleep.

Hot & Not duvet
Are menopausal night sweats creating ‘too hot, too cold’ cover squabbles with your partner? You can customize each half of this duvet to your perfect sleeping temperature.
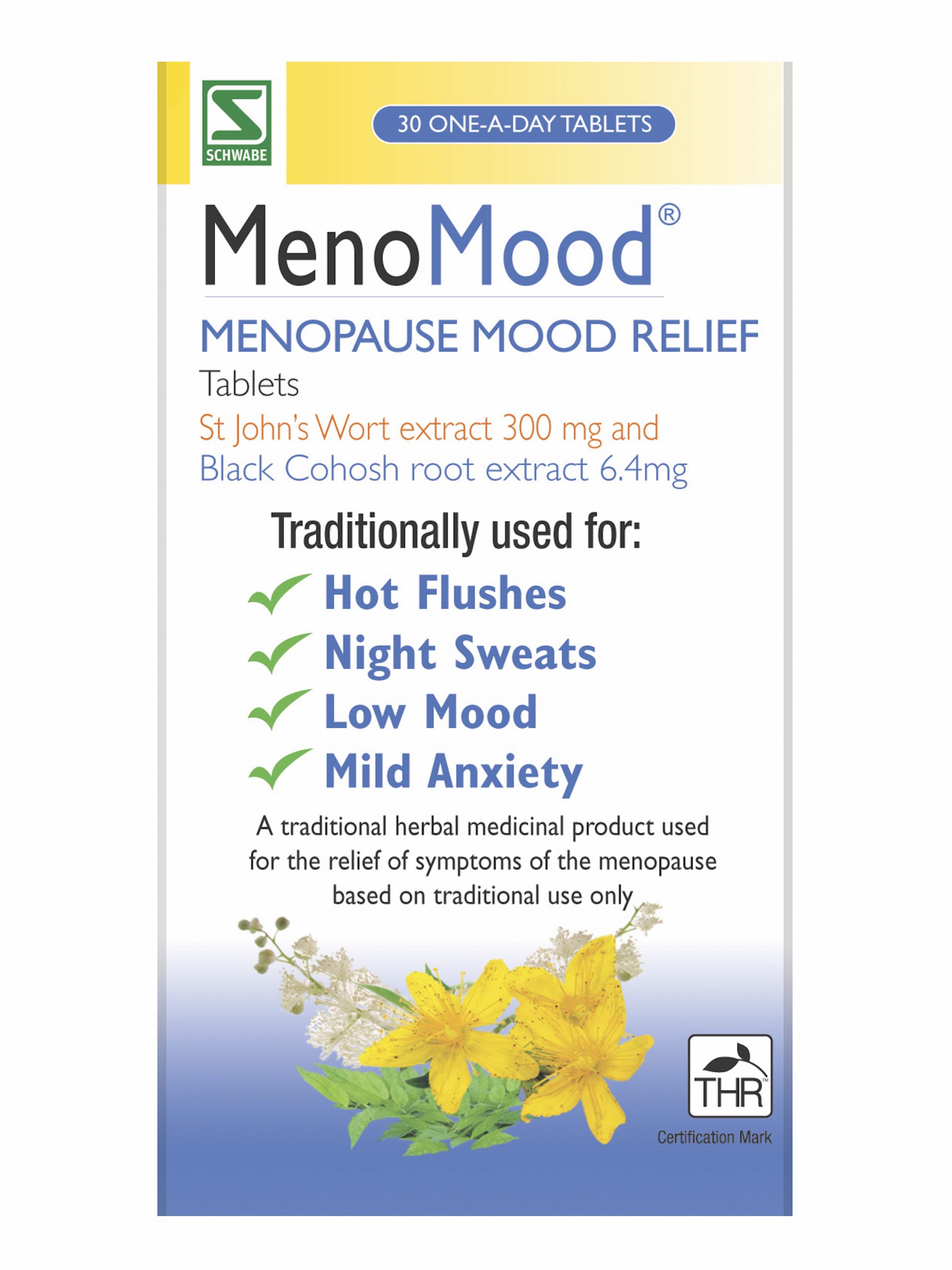
Schwabe Pharma MenoMood tablets
This herbal remedy contains black cohosh to help with hot flushes.
w&h thanks Dr Louise Newson, a GP and author of Menopause (£9.74, Haynes), women’s health specialist Dr Sally Moorcroft, Dr Caroline Houlihan-Burne, clinical hypnotherapist at The Princess Grace Hospital, and clinical psychologist Professor Myra S Hunter, Mark Bovey, head of research at the British Acupuncture Council, for their time and expertise.
Lauren is the former Deputy Digital Editor at woman&home and became a journalist mainly because she enjoys being nosy. With a background in features journalism, Lauren worked on the woman&home brand for four years before going freelance. Before woman&home Lauren worked across a variety of women's lifestyle titles, including GoodTo, Woman's Own, and Woman magazine.
