Health & Wellbeing
Expert advice, tips and guidance from medical and healthcare professionals to help you take care of your physical health and mental wellbeing
Explore Health & Wellbeing
Latest
-

I went for a 30-minute walk every day for a month - here are the surprising benefits I found
Walking 30 minutes a day can do wonders for your health, here's what I learned doing it for a month
By Grace Walsh Last updated
-

I tried running for 30 minutes a day - these are the benefits I found after just two weeks
Writer Samantha Priestley started running 30 minutes a day to boost her physical and mental health. Here are all the changes she noticed in just 2 weeks
By Samantha Priestley Last updated
-

The supplement for maintaining muscle you might not know about (but definitely should)
There are so many benefits of creatine for women. Here, experts explain what it is, how it works, and everything else to expect from the supplement
By Grace Walsh Published
-

Fitbit Premium vs free: What's the difference and is upgrading to Premium worth it in 2024?
Fitbit Premium vs free, which is better? I've tested them both over the last two years, here's the truth about subscribing in 2024 and whether it's worth it
By Grace Walsh Last updated
-

How to boost your energy levels - 5 ways to feel better in under 10 minutes
Wondering how to boost your energy levels without a cup of coffee? These microbreaks may be what you need to feel yourself again in less than 10 minutes
By Debra Waters Published
-

How to do Couch to 5k on a treadmill - 5 steps to complete the beginner-friendly program
Wondering how to do Couch to 5k on a treadmill? Here, a PT reveals the best way to do the program at the gym and all the benefits to be had
By Grace Walsh Published
-

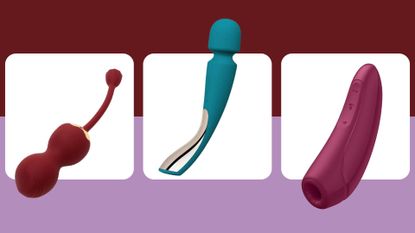
The best rabbit vibrators for first-timers, couples, and those on a budget in 2024
The best rabbit vibrators offer double the stimulation with internal and external arms. Here the w&h health team reveals their tried and tested favourites
By Grace Walsh Last updated
-

Fitbit Sense 2 review: The sleep sensor we've been waiting for
The Fitbit Sense 2 is the latest smartwatch from the brand. Here, Digital Health Editor Grace Walsh reveals whether it's worth buying in 2024
By Grace Walsh Last updated
-

The best Fitbits in 2024 to help you hit your health and wellness goals, tried and tested by our health editor
The best Fitbits can help you reach your goals. Our health editor tried and tested each of the best Fitbits to help you decide on the one for you and your lifestyle
By Grace Walsh Last updated